Overview
Mast cell activation syndrome (MCAS) is a condition which can affect children and adults. Mast cells are a type of white blood cell found in the skin, nerves, lungs and other connective tissues throughout the body. They have the ability to communicate with other immune cells when they detect danger. There are 2 types of mast cells found in the body: mucosal and connective tissue mast cells.
Mucosal mast cells are mostly found in the gut and respiratory tract but can also be found in the blood and connective tissue. They play a key role in the immunity response to bacteria, pathogens, allergic reactions, exposure to toxins, bites, and in response to medications. They offer protection and promote healing when the body is in a healthy state. However, when mast cells function incorrectly, they can cause many disorders with various side effects.¹
Mast cells are created in the bone marrow and are responsible for releasing histamine, which is a chemical that essentially increases blood flow to help the body fight infections. They come in 3 structural forms: intact, spreading, and degranulating. Intact mast cells are those found in the skin and epithelial tissues. Spreading mast cells are found in connective tissues and are less common than intact mast cells. Degranulated mast cells are ones which have released their contents (mediators).
Causes of mast cell activation syndrome (MCAS)
IgE antibodies are present on the outside of the mast cell; when they bind to the allergy-causing proteins, antibody-induced degranulation releases histamine, cytokines, heparin and growth factors. With MCAS, these mediators are too abundant and are considered harmful to the body; they can be triggered by the diet (the gut is home to 70% of the mast cells in the human body), responding to illness, and other external environmental factors. The response is known as ‘systemic’ as it affects a range of systems within the body.4
Mast cell mediators
- Tryptases
- Chymase
- Leukotriene
- Leukotriene C4
- TNF-alpha
- Interleukin 8
- Heparin
- Histamine
- FCER1
- Amines
- Polyamines
- Proteoglycans
- Proteases
- Sulphates
- Cathepsin G
- Phosphoinositide 3-kinase
- Prostaglandins
Primary mast cell activation:
Mast cells can also mutate and produce clones that release these chemicals, resulting in the over-production of these immune mediators, known as ‘primary activation’. These cloned mast cells can form and grow uncontrollably, causing the condition of mastocytosis.¹
Secondary mast cell activation
The mast cell contains many chemicals to help in the immune response, and its mediators are released during exposure to external factors or allergic reactions to reduce inflammation, increase blood flow and destroy pathogens, known as ‘secondary activation’. The viral infection activates mast cells, releasing the pro-inflammatory cytokines that contribute to pulmonary cytokine storms and neurotensin-induced lung inflammation and vascular permeability. ²
MCAS triggers5
- Stress
- Co-infections
- Temperature changes
- Chemicals
- Medications
- Preservatives
- Mould
- Insect bites
- Smells
- Smoke
- Heavy metal toxicity
- Anaesthetic
Idiopathic mast cell activation:
Severe allergic reactions can cause anaphylaxis; in these cases, the patient may experience swelling, hives and difficulty breathing. In these episodes, the cause may be unknown, but there are high levels of mast cell mediators, otherwise known as ‘idiopathic activation’.
Dietary triggers
- Yeast
- Alcohol
- Gluten
- Dairy
- Fermented foods
- Smoked meats
- Shellfish
- Citrus fruits
- Vinegar
- Leftovers
- Berries
Signs and symptoms of mast cell activation syndrome
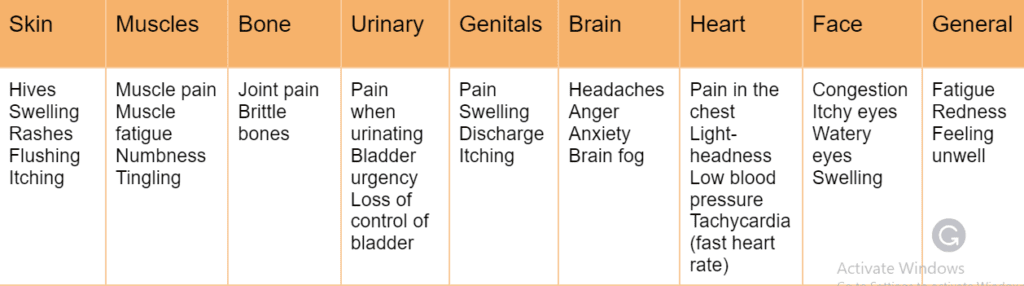
MCAS is a multi-system & multi-symptom chronic condition so signs and symptoms vary on a case-to-case basis. Symptoms come and go over extended periods of time, so recognising the symptoms can be a difficult and lengthy process.
Anaphylaxis is a potentially life-threatening symptom or consequence of MCAS, as with many allergic reactions, you may notice swelling of the tongue, lips and throat. This may be accompanied by difficulty breathing, noticeable wheezing, coughing and feeling faint. These symptoms are serious and require immediate medical attention and the use of adrenaline. If you suffer from anaphylaxis, then you will have EpiPens that are pre-loaded with adrenaline; these must be administered immediately.5
Gastrointestinal symptoms commonly include diarrhoea or constipation, cramping and reflux. Many MCAS sufferers also experience ‘dumping syndrome’ where the food you eat is quickly moved to your small bowel, not allowing food to be digested properly. Symptoms related to gastric dumping include weakness, vertigo, tachycardia (rapid heart rate) and abdominal cramping. This rapid emptying of the stomach can be triggered by food that is low in fibre, high in sugars or simple carbohydrates.5
Respiratory symptoms can involve airway constriction, increased mucus and coughing due to inhalation of aggravators. MCAS sufferers may also suffer from congestion and sinus infections. Mast cells play a key role in allergic asthma, so increased asthma-like symptoms can also be seen in MCAS patients already suffering from asthma.5
Table 1: Additional systemic and general symptoms of mast cell activation syndrome
Management and treatment for mast cell activation syndrome
Managing your symptoms is very important as there is no single cure for MCAS, especially for those who suffer from anaphylaxis. Anaphylaxis is life-threatening and should be treated with epinephrine autoinjectors, followed by care at a hospital.
The other effects of mast cells and mast cell mediators can be treated with antihistamines, stabilisers, inhibitors and aspirin.6
- For cutaneous mastocytosis patients who suffer from inflammation of the skin, steroidal creams can reduce the presence of mast cells in the afflicted area. Oral steroids may be prescribed if you have bone pain or anaphylaxis
- In some cases patients are treated with the drug midostaurin; this medicine can slow the growth of mast cells and improve the overall quality of life for the patient
- Sodium cromoglicate is used for allergy patients; this stabiliser reduces the mediators produced by the mast cells, relieving symptoms such as diarrhoea, conjunctivitis, asthma and food allergies
- Brittle bones (osteoporosis) can be caused by mast cell damage. To slow the damage, bisphosphates and calcium supplements may be prescribed
- Blockers include nilotinib, dasatinib or imatinib
- In extreme cases, chemotherapy may be advised, such as interferon alpha or cladribine
Diagnosis
Early recognition and treatment is key in reducing morbidity; the most frequented diagnostic is by immunologists, with symptoms varying on a case-to-case basis, depending on how the disease manifests and which organ system it affects (Table 1). GP and Nurses should be made aware of the general symptoms associated with MCAS, such as fatigue, generalised malaise, and weight loss, after which you will be directed to a specialist best suited for your symptoms:
- Immunology departments observe nausea, vomiting, flushing, pruritus, urticaria and angioedema. This is the best route for diagnosing MCAS as they are most familiar with the condition. The symptoms they see are due to irritation of the epithelial cells on the inside and outside of the body; endoscopies and colonoscopies are procedures which allow your doctor to observe the internal areas. Tissue and bone marrow biopsies may also be taken, as well as possible genetic testing
- Neurological, Musculoskeletal and pain professionals observe aches, bone pain, osteopenia, osteoporosis, anxiety, depression, decreased concentration and memory, insomnia and migraines. Some of these symptoms are often reflected in other conditions, such as Ehlers-Danlos syndrome (hypermobility) and fibromyalgia (widespread pain), so your doctor may want to investigate bone density and any damage that may have occurred from mast cell-related damage. The only way to see this damage is by bone and CT scans
There is no definite single test for diagnosis of MCAS so the process can take time. Your clinicians will rule out other diagnoses that have similar symptoms, such as Postural Orthostatic Tachycardia syndrome (POTS), type 2 diabetes and other autoimmune conditions. You may be asked to supply urine, blood and stool samples for laboratory analysis to rule out the other causes of your symptoms.
Tryptase is the most reliable biomarker for diagnosis of MCAS; it is detected from the blood samples but must be retrieved within 4 hours of the episode, and repeat blood will be necessary.
Histamine and prostaglandins are also good indicators for MCAS but are not reliable on their own. If you have been directed through the allergy team, you may have to undergo food monitoring, where you keep a diary and monitor when you have flares; this is to understand your triggers. For patients who suffer from anaphylaxis, the main direction is understanding and managing your allergies.
FAQs
Who is at risk of mast cell activation syndrome?
Mast cells respond to toxins, insect bites and allergic reactions. Primary and Secondary MCAS can be triggered following any infection or aggravate an undiagnosed individual. It has been suggested that post and long COVID-19 (SARS-COV2) significantly increases new cases of primary and secondary MCAS.², ³
Who can I talk to
Mast Cell Action is a UK-based charity that offers support to the mast cell disease community, families, doctors and researchers. They offer community support groups on social media for adults who have MCAS and parents of children with MCAS, as well as raising awareness within the medical community for funding and research. Reach out for advice at info@mastcellaction.org.
When should I see a doctor?
With any symptom that is a concern, you should contact your GP; it may help to keep a diary of your symptoms and possible triggers immediately if you are suffering from anaphylactic symptoms.
Summary
Mast cell activation syndromes are an extremely complex group of disorders that affect a wide range of organs. Mast cells are created in the bone marrow and found throughout the body in many different forms. These specialised cells are the first responders to foreign bodies and injury and are a necessity for normal, healthy functioning. However, in many cases, these cells are too sensitive and work too well. Over-stimulation of the protectors leads to over-production of the mediators that help us fight infection and instead cause disease. There are many triggers involved in MCAS, including diet, stress, previous illness and allergic reactions. There are even more symptoms making diagnosis and management of the syndromes very difficult. These symptoms can vary from hives, rashes, ‘dumping’, and widespread pain to severe anaphylaxis and death. There is no one treatment for MCAS, but managing and monitoring your symptoms are key in improving your quality of life. Medications are personalised to your symptoms, from topical steroids to chemotherapy, depending on the severity of the disease. For advice, support and more information, visit www.mastcellaction.org or contact them via email at info@mastcellaction.org.
References
- Mastocytosis [Internet]. NHS; [cited 2023 Jul 21]. Available from: https://www.nhs.uk/conditions/mastocytosis/
- Batiha GES, Al-Quraish HM, Al-Gareeb AI, Welson NN. Pathophysiology of Post-COVID syndromes: a new perspective. Virology Journal [Internet]. 2022 Oct 9 [cited 2023 Jul 3];19(1):158. Available from: https://doi.org/10.1186/s12985-022-01891-2
- Weinstock LB, Brook JB, Walters AS, Goris A, Afrin LB, Molderings GJ. Mast cell activation symptoms are prevalent in Long-COVID. Int J Infect Dis [Internet]. 2021 Nov [cited 2023 Jul 1];112:217–26. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8459548/
- Frieri M. Mast Cell Activation Syndrome. Clin Rev Allergy Immunol. 2018 Jun;54(3):353-365. doi: 10.1007/s12016-015-8487-6. PMID: 25944644.
- Theoharides TC, Valent P, Akin C. Mast Cells, Mastocytosis, and Related Disorders. N Engl J Med. 2015 Jul 9;373:163-172. DOI: 10.1056/NEJMra1409760
- Castells M, Butterfield J. Mast Cell Activation Syndrome and Mastocytosis: Initial Treatment Options and Long-Term Management. J Allergy Clin Immunol Pract. 2019 Apr;7(4):1097-1106. doi: 10.1016/j.jaip.2019.02.002. PMID: 30961835.

 Medical contributor:
Medical contributor: First revision:
First revision:  Second revision:
Second revision: 




