What is Cyanotic Congenital Heart Disease?
Cyanotic Congenital Heart Disease (CCHD) refers to a group of heart defects that are present at the time of birth. These abnormalities occur when one or more parts of the heart fail to form properly during embryonic development. These defects often cause the blood that flows through the body to be under-oxygenated, resulting in a blue-ish skin tint.
In a normally functioning circulatory system, blood returns from its journey through the body to the right side of the heart. This blood is typically low in oxygen, as it passes on this vital molecule to the body’s cells on its path.
This deoxygenated blood then flows back through the heart, where it is pumped into the lungs, and becomes reoxygenated. This oxygen-rich (oxygenated) blood then passes back through the left side of the heart and onto the rest of the body to repeat the cycle.
Those affected by CCHD have various congenital differences in this process that can cause the blood to be perpetually under-oxygenated, oxygenated and deoxygenated blood can begin mixing, and blood may flow less effectively to the lungs.
All of these potential differences result in poorly oxygenated blood, and cause the blue-ish hue in the skin of CCHD sufferers, often referred to as cyanosis.
What are the forms of CCHD?
There are multiple defects that can be classified as CCHD, but some of the most common are Tetralogy of Fallot (TOF), transposition of the great arteries (TGA), and tricuspid atresia.
Tetralogy of Fallot (TOF)
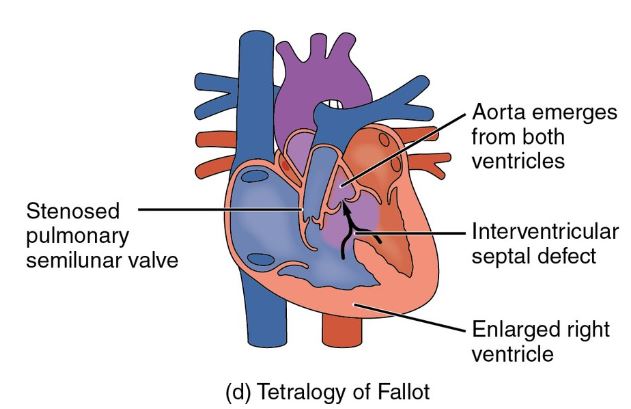
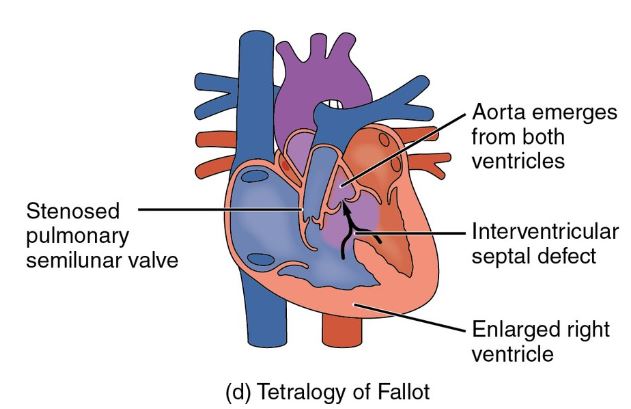
It is the most common form of CCHD and is characterized by a combination of multiple defects, including a hole between the left and right ventricles, a narrow pulmonary valve, thickening of the right ventricle muscles, and a misplaced aortic valve.
The physiology of the heart is a complex series of cycles that keep blood flow consistent, but comprehending each element of TOF can be a key part of understanding CCHD, here is a general breakdown of each defect.
The ventricles of the heart are two chambers made up of strong muscles that forcefully pump blood in and out of the organ.
When a hole is present between these two chambers, deoxygenated and reoxygenated blood may begin mixing, therefore diluting the oxygenation of red blood.
Next, the pulmonary valve is one of several heart valves that is responsible for regulating blood flow through the lungs for reoxygenation. When this valve is especially narrow, blood may flow ineffectively to the lungs, resulting in an under oxygenated blood supply.
Third, when the ventricular muscles are too thick, they may actually block or slow blood flow out of the heart. This process keeps freshly oxygenated blood from replenishing the body’s other organs, therefore slowing their function.
Finally, when the aortic valve is misplaced, it is shifted to the right side of the heart instead of the left, resulting in a mixing of red and blue blood. TOF can be diagnosed as one or multiple of the abnormalities.
Transposition of the great aretries (TGA)
The second most common type of CCHD, TGA, is characterized by a placement switch between the pulmonary and aortic valve. Therefore, low oxygenated blood gets incorrectly pumped back out to the body, where it should pass through the lungs to be reoxygenated.
Tricuspid Atresia
The third most common, tricuspid atresia, occurs when the tricuspid heart valve, a valve that allows the flow of under oxygenated blood into the right ventricle, is damaged or missing entirely. This type of defect disrupts normal blood flow, and allows deoxygenated blood to flow back out to the body.
Although other types of abnormalities may exist, the three described here are the most commonly diagnosed and treated. When the blood supply is not properly reoxygenated as a result of these abnormalities, other organs that rely on the circulatory system can be negatively affected or even forced into organ failure.
Cyanotic vs acyanotic
Cyanotic heart disease refers to any heart defect that negatively affects the presence of oxygen in the blood, such as the defects described above.
If a defect is acyanotic, its existence does not impact the oxygen supply of the body. In these cases, the blue skin tint (cyanosis) is much less common, and may only occur in children during activities that require significant air like feeding or crying.
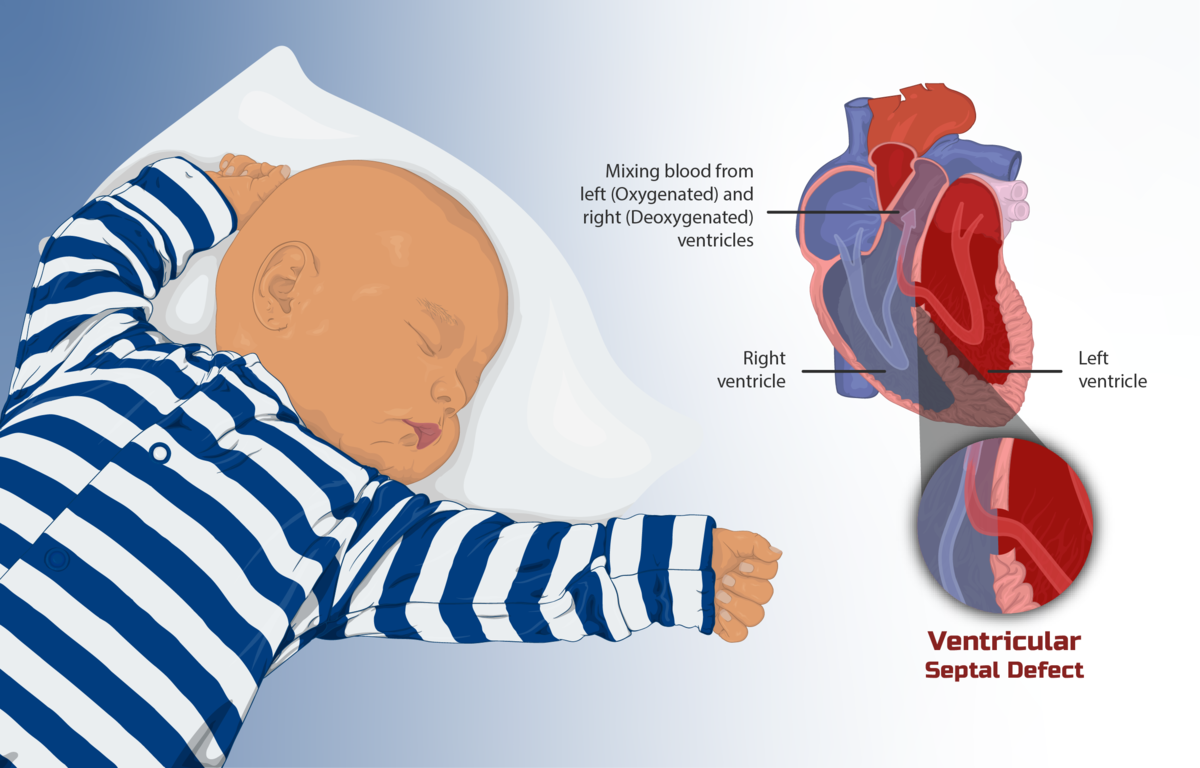
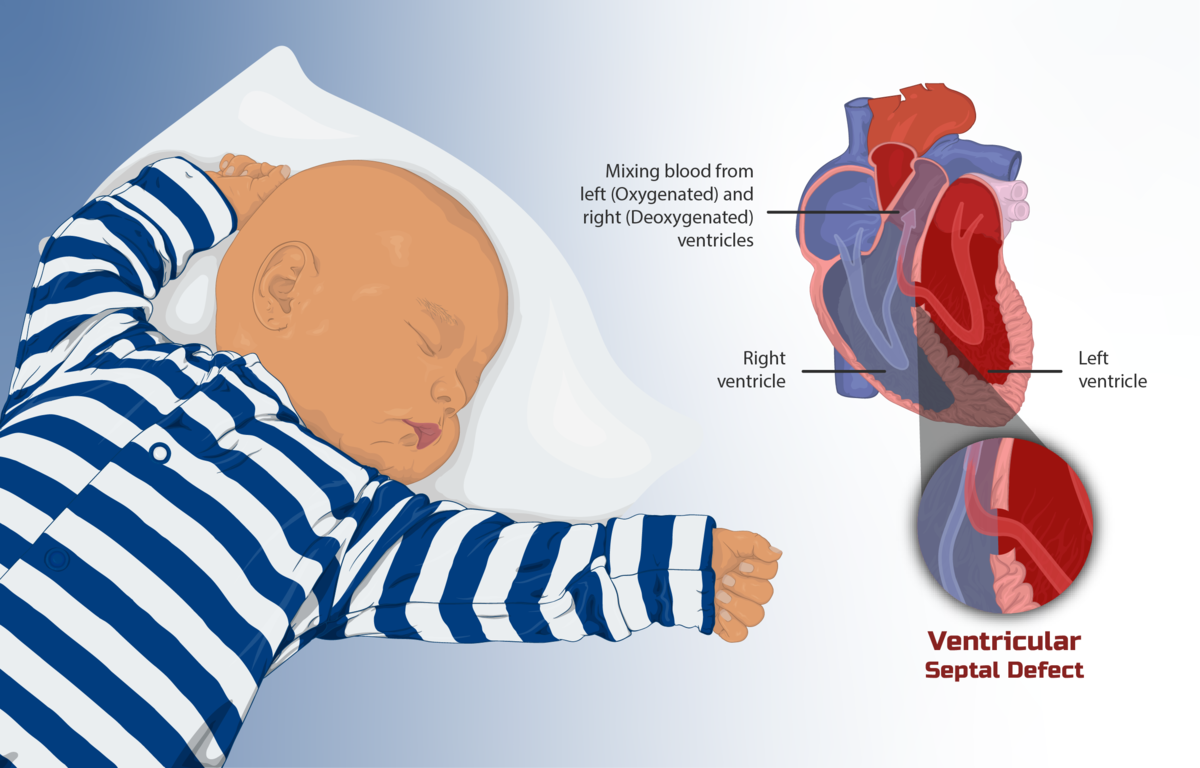
*Image credit by CC BY-SA 3.0, Link
The most common form of acynotic heart disease is ventricular septal defect (VSD), usually diagnosed as a hole between the two lower chambers of the heart. Normally, these holes are very small and never cause symptoms, in some cases, they may even close on their own.
However, in extreme instances, this wall may be entirely missing, in which case the heart struggles to pump enough blood to the body, and too much builds up in the lungs.
The symptoms of acyanotic heart disease usually present themselves within 3 to 6 months of birth, and if required, can be resolved through surgery or a cardiac catheter procedure.
Symptoms
Clubbing
Clubbing is characterized by a swelling of the lower portion of fingers and toes. This swelling occurs when the tissue beneath the nail bed softens, causing fingertips to bulge, and nails to curve.
Nails may appear to “float” instead of being firmly attached, they may also form a very sharp angle with the cuticle, and the swollen fingertip can be red and sensitive.
The biological cause of clubbing is unknown, but it often accompanies various conditions including CCHD. Some evidence suggests that the lack of oxygen in the blood caused by CCHD stimulates the fingers and toes to form extra blood vessels, causing the swelling.
The fingers and toes lie the farthest away from the heart, so when oxygen levels are poor, they suffer the most. Therefore, clubbing may be the body’s attempt to increase oxygen flow to these extremities. There is currently no treatment for clubbing, however, if the underlying condition is remedied the symptom often disappears.
Cyanosis (bluish extremities)
Although mentioned briefly in the section above, cyanosis is a blue skin tint that accompanies low levels of oxygen in the blood supply.
The hue most commonly appears in the lips, tongue, gums, ear, fingers, toes, and under nails, especially after physical activity.
The poorly-oxygenated blue blood can be seen through these locations where the tint appears, typically where the skin is thinnest. In the case of CCHD, the most strenuous activities that stimulate the presence of cyanosis are feeding and crying.
Crying
Crying is a difficult symptom with CCHD, since all babies cry during their first few years of life. However, a baby with CCHD likely struggles to engage in the physical activity of infants, namely feeding. Therefore, a baby suffering from CCHD will cry especially during feeding times, usually accompanied by abnormal sweating as they are overworking themselves to consume food.
This crying also prevents an infant from intaking as much food as is expected and feeding for longer than is normal. Therefore, a parent/clinician should watch for how much formula or breast milk is consumed relative to other babies.
If a baby cannot feed properly, it may also have stunted growth, another indicative sign of CCHD.
Crabbiness
Crabbiness or irritability is very much the same type of symptom as crying. A baby suffering from CCHD is unable to communicate its discomfort and hunger.
Therefore, a parent/ clinician will likely find a baby has difficulty sleeping, cannot relax, and cries without stopping. The infant may not engage in the normal curiosity of other babies, and can appear lethargic or constantly stressed.
Tachycardia
Tachycardia is a clinical term for an extremely fast heart rate, this elevated heart rate can be caused by multiple types of heart arrhythmia.
Arrhythmia is common in those with CCHD as the cycle that creates a heartbeat may be disrupted by various defects. That being said, rapid heartbeat is most commonly observed in babies with TGA.
A fast heart rate is often accompanied by rapid breathing, as the body has to intake more oxygen in order to make up for the limited supply in the blood. This symptom of CCHD is perhaps the most dangerous, as it can lead to heart failure, stroke, or sudden cardiac arrest.
Delayed development
Firstly, a lack of oxygen in the blood may lead to poor development of other organs that rely on this vital function, namely the brain. Without proper oxygen flow, the brain may struggle to develop fully or as quickly as is normal.
Secondly, when a child is experiencing the other symptoms of CCHD, such as irritability or inability to feed, they may also experience delayed development. Either because their brain is not receiving proper nutrition, or because they are not able to engage fully with their environment - a vital part of brain development for a young child.
Finally, an infant with CCHD may spend more time hospitalized or receiving medical treatment, preventing them from having the normal experiences of other children, and undergoing the stresses of an unnatural environment. All of these influences can lead to delayed development in babies suffering from CCHD.
Causes
Tetralogy of Fallot (TOF)
As briefly discussed earlier, TOF is the most common form of CCHD and is usually detected during infancy. The typical defects diagnosed as TOF include a hole between the left and right ventricles, a narrow pulmonary valve, thickening of the right ventricle muscles, and a misplaced aortic valve.
Babies suffering from TOF almost always require corrective surgery, and usually go on to need regular doctor’s visits with some physical activity limitations.
TOF’s causes are mostly unknown, however, its development is likely impacted by:
- viral infections
- alcohol consumption
- poor nutrition
- advanced age during pregnancy.
Furthermore, there appears to be an important genetic component of TOF and a mother with a family history of CCHD. A tell tale sign of TOF is tet spells, or the sudden appearance of cyanosis in the skin. These spells occur most commonly after feeding, when a rapid decrease of oxygen in the blood occurs. Additionally, tet spells are usually spotted between 2-4 months of age.
Transposition of the great arteries
TGA is characterized as a placement switch between the pulmonary and aortic valve. Therefore, unoxygenated blood continues to flow through the body without reaching the lungs, and oxygenated blood becomes trapped perpetually and flows back toward the lungs.
Transposition is often accompanied by other defects, and like TOF, its causes are ambiguous. TGA can usually be detected during prenatal screening, either through an ultrasound or a fetal echocardiogram; however, corrective surgery is often required.
Two types of surgeries are common for babies suffering from TGA, arterial switch operations, and atrial switch operations.
The first surgery simply switches the position of the pulmonary and aortic valve, allowing oxygenated blood flow to return to the body.
The second requires the placement of a tunnel between the atria of the heart so that oxygen- rich blood can pass through the aorta and back through the body.
Tricuspid atresia
Tricuspid atresia occurs when the tricuspid heart valve, a valve that allows the flow of under oxygenated blood into the right ventricle, is damaged or missing entirely. Therefore, blood cannot flow from the right atrium into the right ventricle, and must force its way through another route.
Babies with tricuspid atresia are often also born with a hole between the left and right atria (atrial septal defect), allowing for the mixing of oxygen- rich and oxygen- poor blood supplies.
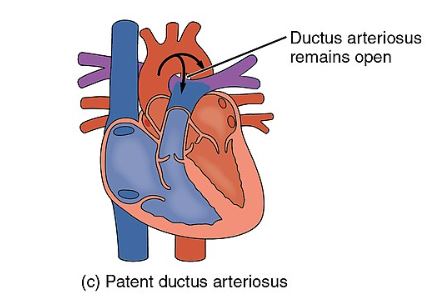
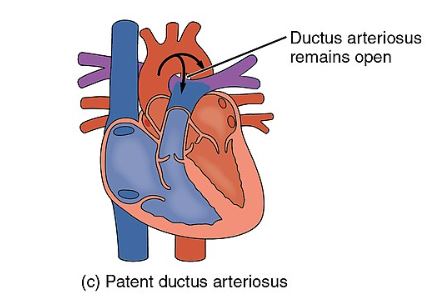
Treatment does not always require surgery, and a doctor may prescribe medication to keep the patent ductus arteriosus (a blood vessel that allows blood to move through the lungs that usually closes after birth) open post-birth. Like other defects, its causes are unknown.
Persistent truncus arteriosus (PTA)
PTA is a particularly rare form of CCHD, and occurs when an embryonic structure called the truncus arteriosus fails to divide into the mature pulmonary trunk and aorta. Therefore, one arterial trunk provides mixed deoxygenated and oxygenated blood to the body instead of deoxygenated blood being directed to the lungs and oxygenated blood out to the rest of the system.
The causes of PTA may be genetic or environmental. PTA requires open-heart surgery with the inclusion of cardiopulmonary bypass, a process by which a medical machine takes over the function of the heart so that the physical organ lays still for operation.
Pulmonary atresia
Pulmonary atresia occurs when the pulmonary valve does not form, causing the body difficulty getting blood to the lungs for oxygenation. In this case, the same medicinal treatment for tricuspid atresia, whereby the patent ductus arteriosus remains open, may be required.
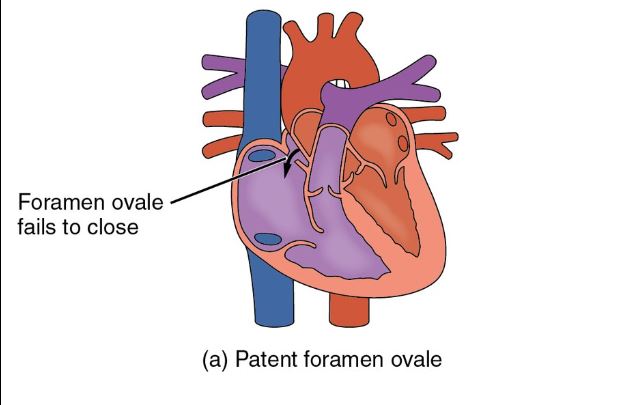
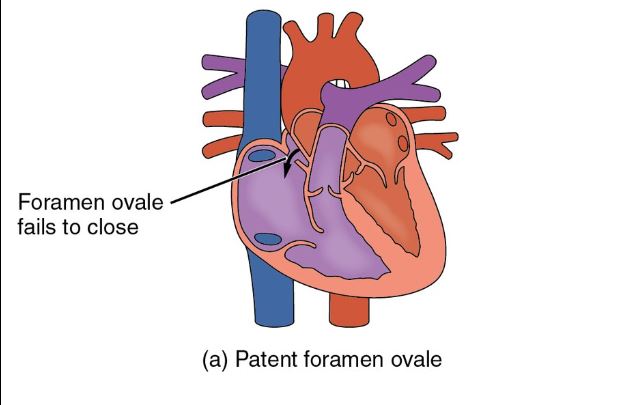
Additionally, the embryonic foramen ovale (a natural opening between the right and left upper chambers of the heart that normally closes after birth) may be forced to remain open via medication. In other cases surgery via cardiac catheterization is required.
Risk Factors
Certain genetic conditions

It’s estimated that 10% of CCHD defects are caused by genetic changes to chromosomes. These changes can be part of a family’s genetic history, or may occur with other chromosomal disorders like down syndrome.
Single gene mutations during embryonic development can potentially limit the production of proteins that later go on to build the heart; these mutations can occur due to environmental factors, although their exact causes are still under scientific investigation.
Maternal diabetes
Women with maternal diabetes are 4 times more likely to have an infant with CCHD. However, the exact biological interaction between maternal diabetes and the generation of fetal heart defects is unknown.
That being said, although diabetes is a complex metabolic disorder with multiple causes, it appears that the characteristic of high blood sugar is likely the culprit for problems associated with embryonic development.
Smoking or drinking during pregnancy
Smoking can cause multiple congenital defects and abnormalities, due to the introduction of serious toxins into the bloodstream that can affect the fetus through the placental barrier.
Rubella during pregnancy
Although the biological interaction between rubella infection and CCHD is ambiguous, it is clear that a woman with rubella is far more likely to have an infant with a heart defect.
Thankfully, the MMR vaccine protects against this type of infection and can protect both a baby and its mother from serious infection-related complications.
Treatment
Most serious forms of CCHD require open-heart surgery to correct blood flow and restore oxygenation.
These surgeries may also be accompanied by cardiac catheterization, and are usually followed by routine doctor’s visits to monitor progress and future development.
These treatments are usually necessary within the first year of life and can be selected after the pulse oximetry screening. This type of screening detects oxygen levels in the blood, whereby a baby either passes a healthy oxygen threshold or fails to indicate the presence of a heart defect.
Some minor defects, especially those that are acyanotic, may not require treatment and can resolve themselves.
However, if a baby is presenting the symptoms of CCHD like rapid breathing/heart rate, cyanosis, or swelling extremities, a doctor should be consulted immediately.
Summary
CCHD is a complex condition with multiple causes, symptoms, and treatment options. However, once corrected, a baby usually goes on to live a normal life developmentally and physically, although long term follow-ups may be necessary. Keeping vigilant, either as a parent or clinician, for the tell-tale signs of congenital heart deformities can allow for quick treatment, and a reduced impact of a low oxygen blood supply.
References:
- Ellis ME. Cyanotic congenital heart disease [Internet]. Healthline. 2018 [cited 2022 Jan 17-23]. Available from: https://www.healthline.com/health/cyanotic-heart-disease
- Cyanotic heart disease [Internet]. [cited 2022 Jan 17-23]. Available from: https://medlineplus.gov/ency/article/001104.htm
- Congenital Heart Defect Types [Internet]. [cited 2022 Jan 17-23]. Available from: https://myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=tx4010
- Ventricular septal defect [Internet]. [cited 2022 Jan 17-23]. Available from: https://myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=stv17232&lang=en-ca
- Talbott JH, Montgomery WR Jr. Familial clubbing of fingers and toes. AMA Arch Intern Med [Internet]. 1953 Nov;92(5):697–700. Available from: http://dx.doi.org/10.1001/archinte.1953.00240230097010
- Hayabuchi Y, Matsuoka S, Akita H, Kuroda Y. Hyperuricaemia in cyanotic congenital heart disease. Eur J Pediatr [Internet]. 1993 Nov;152(11):873–6. Available from: http://dx.doi.org/10.1007/BF01957519
- Sarkar M, Mahesh DM, Madabhavi I. Digital clubbing. Lung India [Internet]. 2012 Oct;29(4):354–62. Available from: http://dx.doi.org/10.4103/0970-2113.102824
- Ossa Galvis MM, Bhakta RT, Tarmahomed A, Mendez MD. Cyanotic Heart Disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29763177
- Mari MA, Cascudo MM, Alchieri JC. Congenital Heart Disease and Impacts on Child Development. Braz J Cardiovasc Surg [Internet]. 2016 Feb;31(1):31–7. Available from: http://dx.doi.org/10.5935/1678-9741.20160001
- Genetic Fact Sheets for Parents - Critical Congenital Heart Disease [Internet]. UK Newborn Screening Laboratory Network (UKNSLN); 2022 [cited 2022 Jan 17-23]. Available from: https://www.newbornscreening.info/Parents/otherdisorders/CCHD.pdf
- Nationwide Children’s Hospital. Influences of maternal diabetes on fetal heart development: High blood sugar during pregnancy is associated with congenital heart defects. Science Daily [Internet]. 2018 Dec 21 [cited 2022 Jan 17-23]; Available from: https://www.sciencedaily.com/releases/2018/12/181221142509.htm
- Simeone RM, Devine OJ, Marcinkevage JA, Gilboa SM, Razzaghi H, Bardenheier BH, et al. Diabetes and congenital heart defects: a systematic review, meta-analysis, and modeling project. Am J Prev Med [Internet]. 2015 Feb;48(2):195–204. Available from: http://dx.doi.org/10.1016/j.amepre.2014.09.002
- Correa A, Levis DM, Tinker SC, Cragan JD. Maternal cigarette smoking and congenital heart defects. J Pediatr [Internet]. 2015 Apr;166(4):801–4. Available from: http://dx.doi.org/10.1016/j.jpeds.2015.01.013
- Factors that may lead to a congenital heart defect (CHD) [Internet]. [cited 2022 Jan 17-23]. Available from: https://www.stanfordchildrens.org/en/topic/default?id=factors-contributing-to-congenital-heart-disease-90-P0178814.






